Plantar Fasciopathy/ Fasciitis: Heel Pain
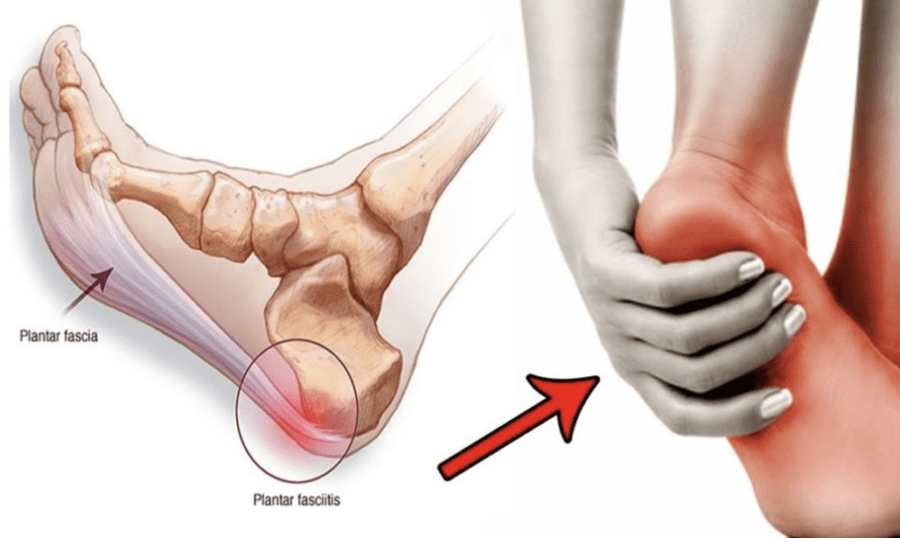
What is Plantar Fasciitis?
One of the most prevalent causes of heel pain is plantar fasciitis (PLAN-tur fas-e-I-tis). It is caused by inflammation of a broad band of tissue that links your heel bone to your toes and runs across the bottom of your foot (plantar fascia).
Plantar fasciitis is a type of plantar fasciitis that causes stabbing pain when you take your first steps in the morning. The discomfort usually goes away as you get up and move around, but it may come back after long periods of standing or when you stand up after sitting.
Runners are more likely to get plantar fasciitis. Plantar fasciitis is more common in overweight people and people who use shoes with insufficient support.
Symptoms
Plantar fasciitis creates a stabbing pain near the heel on the bottom of your foot. The discomfort is normally the severe when you take your first few steps after waking up, but it can also be caused by long periods of standing or getting up after sitting. Exercise generally makes the pain worse, not during it.
New patients at our clinic are often confused by the overwhelming information posted on the internet. Much of the treatment advice for Plantar Fascitis/Fasciopathy is conflicting and produces varied results.
We refer to this information source as Dr. Google and we are all guilty of knocking on his door when a part of our body hurts. The problem is that what works for one person, won’t necessarily work for another. As human beings we are all different and in particular our feet are different. There are 26 bones and 34 joints in one foot so the chances of one foot being the same as another is pretty slim. Even 2 feet that belong to the same person will have subtle differences!
The fact that people's feet function differently will probably explain why the cause of Plantar Fasciitis in one person will be different from the cause of Plantar Fasciitis in another. And let’s face it, there are several causes of Plantar Fasciitis so a “one size fits all” treatment approach is naïve.
If your friend or work colleague hears of your Heel Pain and offers, “ I had Plantar Fasciitis once, just buy some arch supports from the Pharmacy” or “ I had a Heel Spur once, just roll your foot on a tennis ball”, you shouldn’t be surprised if your pain doesn’t go away. There are so many variables that need to be considered, fundamentally – what is the cause of the condition in your particular foot.
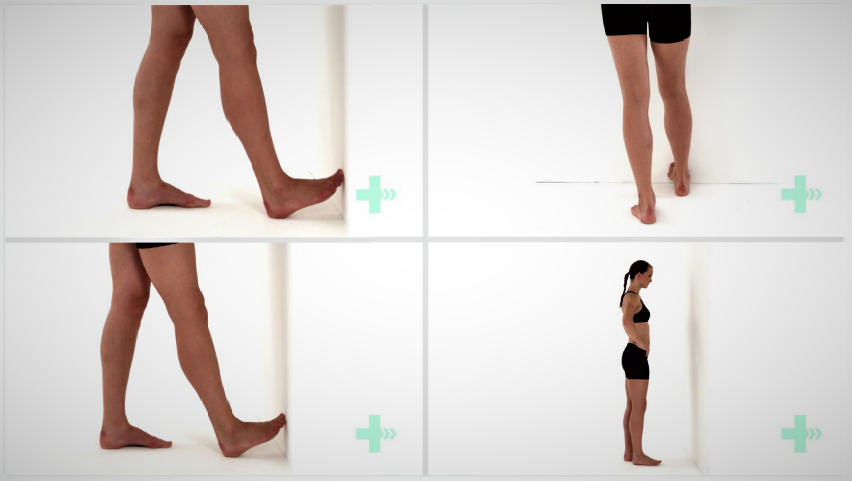
As a Sports Podiatrist & Physiotherapist Team, this is where I come in. It’s our job to analyse you and investigate and find that cause. We use cameras to video your feet, we look at you walking on a treadmill, we use pressure plate to do the pressure mapping of your feet when walking, we take foot measurements and look at joints and muscle range.
We pay particular attention to footwear too as I understand that patients have no idea what sort of footwear are suitable for their feet. It’s understandable – why would you know which shoes match your foot type unless you were experienced in this area.
So it’s no surprise to me when I see a new patient with Plantar Fasciitis who has been wearing ballet flats and scuffs when they have tight calves and flat feet.
The point I’m trying to make here is that unless you know what has caused your Plantar Fasciitis or HeelPain, and you are able to remove that cause, then you are probably not going to resolve your condition. If the lady with the flat feet and tight calves in the ballet flats, keeps rolling her heel over a frozen coke can, but continues wearing the ballet flats and doesn’t address the tight calves, then she is wasting her time.
I do understand why patients call our clinic and ask the question “So how will you treat my Heel Pain, I’ve got Plantar Fasciitis?” but there is not one answer. In fact, the short answer is “ I don’t know because I haven’t seen you yet” and the reality is that I need to assess you to find the cause. Once I have seen a patient I then remove the cause and implement treatments to unload the fascia and accelerate healing. It sounds simple, and in a way it is. Most patients find it simple too, once explained.
I hope this helps to explain why Dr. Google isn’t always able to help you as he has others with the same problem, and that in order to successfully treat your Plantar Fasciitis it is important to find the cause.
If you want to run but are worried about developing OA, a physiotherapist can examine your risk factors and discuss the benefits and drawbacks of running for you as an individual. They can assist you in developing a specific plan and techniques to help you avoid injury, such as strength and conditioning programmes or relaxing stiff joints and muscles, and they can also assist you in properly rehabilitating injuries if they do occur.
EXERCISES FOR PLANTAR FASCIITIS
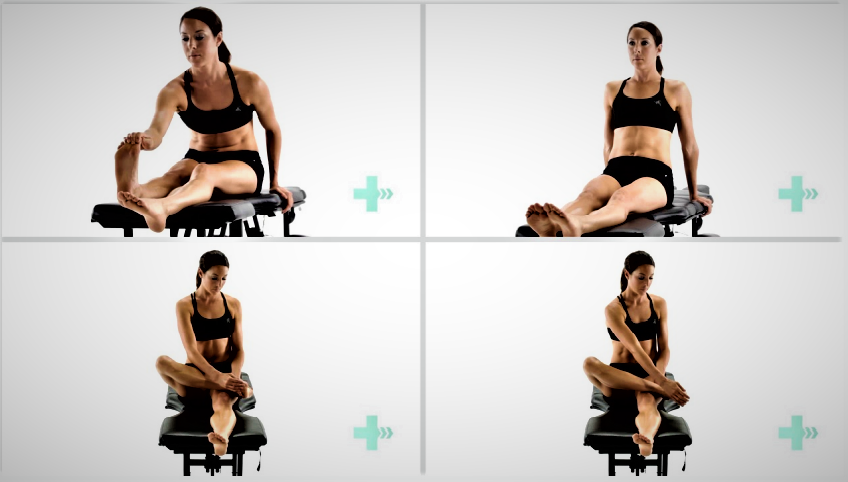
Plantar fascia stretch
3 Sets / 5 Reps
Start in a seated position with your legs extended. Reach down and grab your toes. Pull back on the toes, the big toe especially until you feel a stretch in the arch of the foot. Alternatively, if you are not so flexible, take your leg and cross it over your knee. Grab onto your toes, pulling the big toe back towards you, feeling the stretch in the arch of the foot.
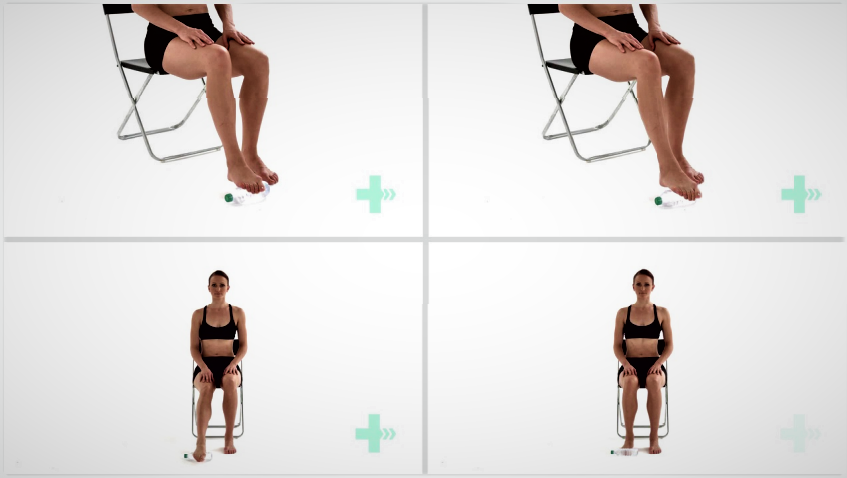
2. Water Bottle PIantar fascia stretch
3 Sets / 5 Reps / 20 sec duration
Take a hard plastic bottle. Place the bottle on the floor under the sole of your foot. Slightly press your foot against the bottle and roll it forwards and backwards.
3. Toe extension stretch against wall
2 Sets / 5 Reps / 20s hold
Place the toes of you affected leg up against a wall. Keeping your heel in contact with the floor and your knee bent, push your knee forwards towards the wall. Hold this position, relax and repeat. You will feel the stretch through the lower calf and sole of your foot.
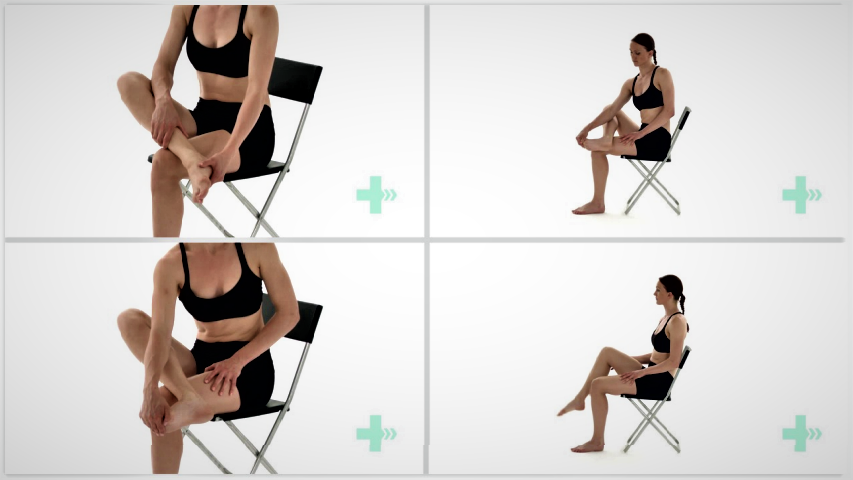
4. Plantar fascia stretch sitting
3 Sets / 5 Reps / 10s hold
Sit up straight in a chair. Place the ankle of your affected leg over the knee of your other leg. Grasp the toes of your affected foot and pull your foot and toes up towards you. You should feel a stretch in the sole of your foot. Hold this position.
Contact us: 0121 285 5656 Email: hello@thepodiatryclinics.co.uk
OR simply click the button below!